Newsroom
Our latest news and
announcements.

Does dry shampoo increase cancer risk?
Dry shampoo can be a lifesaver - a quick spray on busy mornings, after the gym, or when there’s just no time to wash your hair. But recent concerns about safety have left many people wondering: is it actually safe to use?
Is dry shampoo bad for your health?
Dry shampoo, in itself, isn’t known to be harmful. The worry started when small amounts of benzene - a chemical linked to cancer - were found in a few aerosol products. Benzene is classed as a known carcinogen, but the risk comes from high levels over long periods, often in industrial settings. That’s very different from occasional use at home.
In 2022, independent testing picked up very low levels of benzene in some batches of aerosol personal care products - including a few dry shampoos. As a precaution, those products were recalled. These recalls weren’t triggered by anyone developing cancer - they were a safety-first move. And it was only certain batches, not all dry shampoos.
What is the cancer risk from using dry shampoo?
The evidence so far suggests the cancer risk from using dry shampoo is extremely low for most people. Most of what we know about benzene and cancer comes from:
- Long-term, high-level exposure
- Daily contact in certain jobs
- Years of repeated exposure
That’s not the kind of contact people usually have with dry shampoo.
Is there a link between dry shampoo and cancer?
There’s no need to worry if you’ve been using dry shampoo - but here’s what you can do if you’re still concerned:
- Check your product to see if it was part of a recall
- Use sprays in a well-ventilated space to reduce any potential exposure
- Choose non-aerosol alternatives if you’d prefer to avoid sprays
If your product wasn’t recalled, there’s no evidence that it’s unsafe.
The current research does not show a clear link between dry shampoo use and cancer. The concerns relate specifically to trace benzene in certain spray products - and even then, the risk is thought to be very low. It’s always okay to ask questions about your health. And it’s also okay to want reassurance about everyday products.

Is peanut butter linked to cancer?
Peanut butter has had a lot of bad press - and not always fairly. It’s one of those foods that often pops up in cancer myths. So let’s clear things up. There’s no good evidence that peanut butter causes cancer.
Where did the cancer myth come from?
The worry comes from something called aflatoxins - natural toxins produced by certain moulds that can grow on peanuts if they’re stored in warm, humid places. Long-term exposure to high levels of aflatoxins has been linked to liver cancer, but this mostly applies to parts of the world where food safety systems aren’t strong or consistent.
In places like the UK, Europe, and the US, strict food standards are in place. Peanuts and peanut butter are carefully tested and monitored to make sure aflatoxin levels stay well below anything that could cause harm. So, if you’re picking up a jar from your local shop, there’s no need to worry.
Is peanut butter safe to eat?
Yes! Better yet, it can even be part of a healthy, balanced diet. Peanuts are full of nutrients: protein, healthy fats, fibre, and antioxidants. Studies haven’t shown any consistent link between eating peanut butter and an increased risk of cancer. That said, peanut butter is calorie-dense. Like many delicious things, it’s best enjoyed in moderation - especially as weight gain and obesity are known cancer risk factors.
Whether it’s organic, crunchy, smooth, or straight from the spoon - all commercial peanut butters sold in regulated markets must meet the same food safety standards. If you’re buying from trusted retailers, your peanut butter has been through rigorous checks, regardless of the label. Choosing natural or no-added-sugar versions can help if you’re watching your sugar or salt intake. But when it comes to aflatoxins or cancer risk, there’s no extra concern.
So, should I worry about peanut butter?
Peanut butter isn’t something most people need to fear. If you’re buying from reputable shops in countries with strong food regulations, it’s been checked, tested, and cleared for safety. Like many everyday foods, it’s about context and balance. Peanut butter on toast isn’t a risk - it’s a snack.
What matters more is your overall lifestyle, your health as a whole, and how you feel in your own body. If you ever notice a change that doesn’t feel right - whether it’s with food, digestion, or anything else - it’s always worth speaking to a doctor. The earlier something’s spotted, the more options you’ll have.
Food and health can feel overwhelming, especially with so many myths out there. But when it comes to peanut butter, there’s no reason for fear. Just good sense, solid science, and perhaps one less thing to worry about in your kitchen cupboard.

Do smart watches or wearables pose any cancer risk?
Smart watches and fitness trackers are designed to be worn close to the body, often all day. They sit on the skin, collect health information, and connect wirelessly to phones.
Because of that constant contact, it’s understandable to wonder whether they could affect cancer risk over time.
The question usually comes back to the signals they use to communicate.
What kind of signals these devices use
Wearable devices use low-power radiofrequency signals, most commonly through Bluetooth. These signals are non-ionising. That means they do not damage DNA in the way radiation from X-rays or scans can.
When researchers measure how much of this energy is absorbed by the body, the levels are very low. They sit well below international safety limits that are set to avoid known biological effects. The exposure is also much lower than that from a mobile phone.
In the medical literature, wearable devices are not flagged as a cancer concern. Research focuses on how they can be used safely in healthcare - including in cancer care - without evidence of harm linked to their everyday use.
Why the information can feel unsettling
You may see radiofrequency fields described as “possibly carcinogenic” by international agencies.
This label reflects uncertainty, not proof. It is based on a wide range of exposures, many of them much higher or very different from what consumer wearables produce.
At the levels generated by smart watches and fitness trackers, reviews of the evidence have not identified a credible way these signals would lead to cancer. Regulatory bodies have not issued warnings about cancer risk from wearable devices.
What tends to come up in real life
When clinicians see problems linked to wearables, they are usually local and practical.
Most involve the skin. Irritation, pressure marks, or contact allergy from straps or materials are the common issues, particularly if a device is worn tightly or without breaks.
If a skin change under a device doesn’t settle after removing it for a while, it’s reasonable to show it to a clinician. That’s because ongoing skin changes are worth checking on their own terms, not because cancer is expected.
Based on what we know, smart watches and wearable devices do not appear to increase cancer risk.
Questions like this matter because people pay attention to what they live with every day. Understanding the evidence can replace background worry with context. Earlier understanding isn’t about alarm. It gives people more clarity, more choice, and more ease in asking questions when something doesn’t feel right.
References
Guido K, Kiourti A. Wireless Wearables and Implants: A Dosimetry Review. Bioelectromagnetics, 2020.
Fonseka LN, Woo BK. Consumer Wearables and the Integration of New Objective Measures in Oncology. JMIR mHealth and uHealth, 2021.
Beg S, Handa M, Shukla R, et al. Wearable Smart Devices in Cancer Diagnosis and Remote Clinical Trial Monitoring. Drug Discovery Today, 2022.
Triantafyllidis A, Kondylakis H, Katehakis D, et al. Smartwatch Interventions in Healthcare: A Systematic Review. International Journal of Medical Informatics, 2024.
Featured
Why every moment matters: A message from Dr Miles Payling
At the inaugural C the Signs Conference, Dr Miles Payling - Co-Founder and Chief Scientific Officer - delivered a message that captured the heart of a movement reshaping how the world detects cancer.
He spoke about science, yes. But more importantly, he spoke about people. About time. About the moments we can give back when cancer is found sooner.
“We can’t afford to wait for symptoms to become obvious. Every moment matters - because every moment lost is a choice, a treatment, a life that could have been saved.”
The question that changed everything
Miles shared the story that shaped the mission behind C the Signs.
As an NHS doctor, he met a patient named Joe - active, fit, and 60 years old. After several GP (primary care) visits with vague symptoms, Joe arrived at hospital jaundiced and unwell. Scans confirmed metastatic pancreatic cancer.
Three weeks later, Joe died.
“Joe never asked, why do I have cancer? What he asked was, why was my cancer picked up so late?”
That question became the foundation of C the Signs - a platform built to help clinicians detect cancer early enough to change the outcome.
Today, that vision makes a measurable difference: a patient with cancer detected every 22 minutes.
Each one represents a life identified sooner - and a future that’s less defined by fear.
Why early detection still falls short
Cancer remains one of the leading causes of death worldwide. Survival still depends heavily on the stage at diagnosis.
- Breast cancer five-year survival falls from 97.9% at stage 1 to 26.2% at stage 4.
- Bowel cancer falls from 91.7% to 10.3%.
- Yet only around 58% of patients are diagnosed at an early stage.
In primary care - where most people first seek help - clinicians face enormous pressures:
brief consultations, complex presentations, thousands of patients, and on average only a handful of cancer diagnoses each year. As Miles said in his conference speech:
“The problem isn’t people. It’s knowledge. We need to give every GP the power of precision - instantly.”
Early detection doesn’t fail because clinicians aren’t trying.It fails because cancer is complex, symptoms are subtle, and the time to make sense of them is short. Our platform exists to bridge that gap - offering clinicians timely clarity when decisions need to be made.
Innovation and redefining what’s possible
C the Signs brings together trusted medical evidence, real-time data and AI-powered insight to support clinicians in moments where clarity matters most.
Within seconds, our platform can highlight when a patient may be at risk and guide their doctor toward the right diagnostic pathway - across more than 100 cancer types. But the impact isn’t defined by speed, it’s defined by the lives reached sooner.
Real-world evaluations across the NHS have shown that clinicians using C the Signs are able to:
- identify patients whose symptoms signal concern - even when the signs are hard to spot
- offer reassurance by safely ruling out risk when symptoms are more likely to be benign
- give clinicians clearer insight into where a tumour may have started
- help reduce emergency cancer presentations by half
- shorten the time it takes for patients to reach a diagnosis
Each of these outcomes represents something deeply human: a patient receiving answers earlier,
a family spared uncertainty, a healthcare system given space to care, not catch up.
This is what innovation should do - not stand in the place of clinical judgement, but enhance it. It should deepen insight and make the subtle more visible, so clinicians can act early with the confidence their patients deserve.
The movement, and honouring Jess’s Rule
Miles closed by sharing the story of Jessica Brady - a 27-year-old whose symptoms were subtle, persistent and easy to misinterpret. Despite several visits to her doctor, her cancer was found too late. Her loss is felt deeply, not only by those who loved her, but by clinicians across the country who want every patient to be seen in time.
To honour her legacy, our team is introducing Jess’s Rule - a safeguard within the platform that gently alerts clinicians when a patient returns multiple times with unresolved symptoms, prompting a thoughtful, timely cancer risk assessment.
It’s a small change with a profound purpose: to make sure no patient is ever unintentionally overlooked, and no pattern is missed simply because symptoms are subtle.
As Miles said:
“We can turn tragedy into transformation - by ensuring that no patient is ever overlooked again.”
Jess’s story is a reminder of why this movement matters. Together, we can help make early cancer detection a standard for everyone - not a privilege for a few - and give each person the time, choice and hope they deserve.
News
.png)
Northamptonshire embraces earlier cancer detection
Northamptonshire ICB, in partnership with East Midlands Cancer Alliance, have taken an important step towards earlier, more equitable cancer diagnosis - bringing C the Signs to every GP practice across the county.
This move follows strong demand from clinicians across Primary Care, many of whom asked for extra support in spotting cancer earlier and gaining clearer guidance when symptoms are hard to interpret. It reflects a shared commitment across the county: to give patients the best chance of being seen, understood, and referred in time.
Listening to clinicians, supporting patients
In busy GP practices, symptoms can be subtle, overlap with everyday conditions, or appear gradually over time. It’s easy for patients - and even experienced clinicians - to feel uncertain.
Northamptonshire ICB heard repeated calls for a system that could bring together complex information, reduce the burden of manual processes, and offer an extra layer of safety and clarity. With C the Signs now in place, clinicians have consistent, integrated support to help identify risk earlier across more than 100 cancer types.
Championing early diagnosis across the county
This rollout has been shaped by local clinical leaders who have long advocated for reducing variation in early cancer detection.
Dr Azhar Ali, Clinical Lead for Cancer at Northamptonshire ICB, shared his hope for what this will mean for patients and families across the region:
“With C the Signs in place, we can reduce any variation of early cancer detection irrespective of where they live within Northamptonshire. As an ICB, we are committed to a stage shift to more cancers being detected at stages 1 & 2 and therefore reaching better outcomes for patients.”
Dr Catherine Massey, Clinical Director at Grand Union PCN, highlighted how additional safety and clarity can support busy primary care teams:
“We’ve had some significant events in the past where two-week-waits were missed. C the Signs is a safe system that stops these near misses, and makes decision-making as a GP easier and safer.”
Their leadership has helped shape an implementation that meets the needs of both clinicians and patients.
A shared commitment to earlier diagnosis
The Northamptonshire rollout marks a significant moment for the region and for the national movement towards earlier cancer detection.
It shows what is possible when clinicians speak up for what they need, and when systems listen. It shows the value of giving every patient - in every community - the same chance of being seen early, and it shows the power of combining clinical expertise with technology designed to support, not replace, the human judgement at the heart of Primary Care.

How AI technology can help with early cancer detection in the NHS
A new study presented at the ASCO Care Quality Symposium 2025 and published in the Journal of Clinical Oncology (JCO Oncology Practice) has shown that C the Signs, an artificial intelligence (AI) platform supporting earlier cancer diagnosis, has delivered an 808% return on investment (ROI) for the NHS.
Commissioned by Health Innovation East, the independent evaluation found that implementation of C the Signs across Suffolk and North East Essex Integrated Care Board (ICB) was associated with 272 patients being diagnosed earlier and £1.5 million in annual cost savings - demonstrating how AI can help improve patient outcomes and optimise NHS resources.
By helping GPs identify patients at risk of cancer sooner and reduce unnecessary urgent suspected cancer (USC) referrals, the platform has also eased system pressures and released valuable clinical capacity across the region.
“This study provides clear evidence that AI can make a measurable impact on cancer care,” saidDr Miles Payling, Chief Scientific Officer at C the Signs. He went on to say:
"An 800% return on investment means we’re improving early diagnosis and helping the NHS use its resources more efficiently. It’s a practical example of innovation making care better for both patients and clinicians.”
The study builds on earlier research, also published in JCO Oncology Practice and presented at ASCO, which found that GP practices using C the Signs achieved a 12% increase in cancer detection rates - from 58.7% to 66.0% - without increasing referral activity.

Together, these studies show that C the Signs helps detect more cancers at an earlier stage while maintaining stable referral volumes - supporting NHS priorities around early diagnosis, productivity, and elective recovery.
“Early diagnosis gives patients the best chance of successful treatment,” said Dr Seema Dadhania, Clinical Oncologist at Imperial College London and author of the study. Dr Dadhania further stated:
“C the Signs is helping primary care clinicians identify those subtle cancer presentations that can otherwise be missed - improving detection while reducing unnecessary referrals. It’s a model for sustainable early diagnosis.”
Scaling Across the East of England
Following the success in Suffolk and North East Essex, Health Innovation East has supported the expansion of C the Signs across Norfolk and Waveney ICB, with further rollouts planned across the East of England.
Piers Ricketts, Chief Executive at Health Innovation East said:
“This work is a strong example of technology delivering measurable benefit. C the Signs has shown that AI can help clinicians find cancer earlier.
He continued: "This is of obvious benefits to patients whilst also easing the pressure on NHS services, in particular on primary care. The results from Suffolk and North East Essex are a real success story for innovation in the NHS and show how the service can progress towards its goal of increasing early detection rates from 50% to 75% by 2028.”
Dr Peter Holloway, GP Partner at Mendlesham Practice, Cancer Lead for Suffolk and North East Essex ICB, Chair of the Primary Care Group for the East of England Cancer Alliance, and Cancer Research UK GP for the East of England said:
“The NHS has set an ambitious target to achieve 75 percent early stage cancer diagnoses by 2028. To reach this, we must strengthen primary care’s ability to recognise early symptoms of cancer and ensure timely investigation and referral. C the Signs – a clinical decision support system integrated seamlessly within GP IT systems – helps deliver on these objectives.
Shedding further light on the impact, Dr Holloway said: "Research has shown a 12 percent increase in cancer detection rates in Ipswich and East Suffolk following its implementation. Moreover, it demonstrates a strong return on investment: by ensuring patients are quickly directed to the right pathway, the system effectively pays for itself and reinforces the value of a digital first approach.”
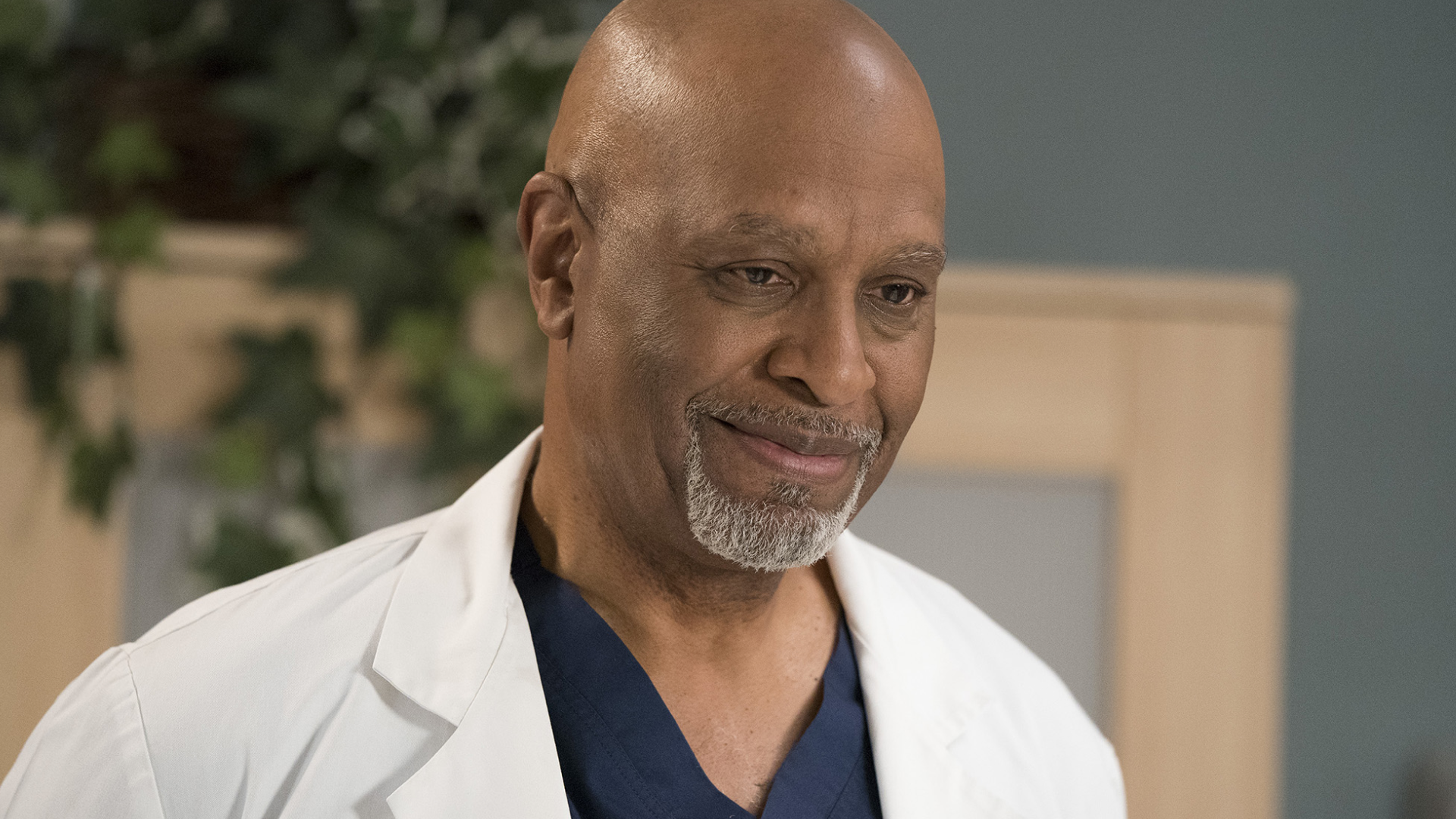
How early prostate cancer detection helped James Pickens Jr. get more time
Actor James Pickens Jr., known to millions for his role as Dr Richard Webber on Grey’s Anatomy, has shared his personal experience with prostate cancer - a decision he hopes will encourage more men, especially Black men, to understand their risk and speak to a health professional sooner.
Pickens, now 73, was diagnosed after his annual physical in 2024. For him, the news was not entirely unexpected. Prostate cancer has affected many men in his family across generations. That family history meant he was diligent about monitoring his health - something that ultimately made all the difference.
“My urologist said it worked in my favour,” he shared.
“Because I was so consistent with my testing, they were able to catch it early.”
During his check-up, elevated PSA levels led to a referral to a urologist. A biopsy confirmed a tumour, and a PET scan showed it hadn’t spread. Given his early diagnosis, Pickens was able to choose between radiation or surgery. He opted for a robotic prostatectomy, supported by a team who kept a close eye on a rare cancer variant found during testing.
“They told me they hadn’t seen one detected as early as mine,” he said - a powerful reminder of what’s possible when cancer is identified in time.
Pickens has spoken openly about the stigma that often surrounds men’s health, especially conversations about prostate cancer. Many men delay seeking help, feel uncertain about what’s normal, or worry about “making a fuss”. These barriers are even more pronounced for Black men, who face a higher risk due to genetic and structural factors.
“One in eight men will be diagnosed with prostate cancer,” he said in a recent public message. “For Black men, the risk is even higher. His story reinforces a truth we hear across healthcare: the earlier prostate cancer is detected, the more options men have - and the better their outcomes can be.
"Early detection is key, and sometimes there are no noticeable symptoms.”
How do you know if you have prostate cancer?
Prostate cancer can be difficult to recognise in its early stages - not because people aren’t paying attention, but because the body often gives very few clues at the beginning. That’s why understanding your own baseline, your personal risk, and what feels normal for you is so important.
There isn’t one single sign to look out for. Instead, there are moments worth pausing on - small changes, shifts in how your body behaves, or a sense that something simply feels different.
You don’t need to be certain something is wrong before speaking to a doctor. You just need to notice a change.
For many men, that might look like:
- A change in the way you urinate - starting, stopping, or feeling different
- Going more often, especially at night
- A stream that feels weaker or slower than usual
- A lingering sense that your bladder hasn’t fully emptied
- Or simply a feeling that something isn’t quite your normal
These changes don’t automatically mean prostate cancer. They’re far more often caused by benign prostate enlargement - a common part of ageing. But they are still worth a conversation, because the earlier any prostate issue is understood, the more options you have.
Your risk also changes over time. Growing older, having Black heritage, or having a family history of prostate, breast or ovarian cancer can increase the chance of developing prostate cancer - which is why some people choose to check in sooner.
A doctor may talk to you about a PSA blood test - a simple blood test that measures the level of prostate-specific antigen - a protein made by the prostate. It isn’t a diagnosis, and it doesn’t give all the answers - but it can offer a helpful starting point if you want to understand your risk more clearly.
What matters most is listening to your body. You know when something feels different. And you deserve to be taken seriously, to ask questions freely, and to have the right support at the right time.

MP Joe Powell C's the Signs in Kensington
Earlier this month, Joe Powell, Member of Parliament for Kensington and Bayswater, visited Golborne Medical Centre to see how local GPs are using C the Signs.
Hosted by Dr Meena Nathan and Dr Thushara Goonewardene, the visit brought together community clinicians, C the Signs Co-Founder Dr Miles Payling, and local leaders to explore how innovation, teamwork, and community engagement are transforming early diagnosis in one of London’s most diverse communities.
Transforming Early Diagnosis in Primary Care
Inside the busy surgery, clinicians demonstrated how C the Signs supports decision-making in real time - analysing patient records, symptoms, and risk factors to surface hidden indicators of cancer during routine appointments.
“We’re still early in the rollout, but already it’s helping us prioritise patients who might otherwise slip through the cracks,” one clinician shared.
C the Signs’ AI models - validated across more than 500,000 patient records - have achieved 99% sensitivity for cancer detection and 94% accuracy in predicting tumour origin. In real-world NHS evaluations, practices using C the Signs have seen a 50% reduction in emergency cancer diagnoses and a 20–50% improvement in time to diagnosis.
Discussions during the visit focused on addressing barriers such as low screening uptake and under-detection in harder-to-spot cancers like pancreatic and lung - areas where C the Signs’ AI-driven case finding is already being deployed across the NHS.
Community, Compassion and Continuity
Beyond technology, clinicians emphasised the human side of early diagnosis. One GP described how her team intervened when a patient’s surgery was nearly cancelled due to language barriers:
“She came in completely distraught. We stepped in, made the calls, got her rebooked. That kind of support takes time - but it changes everything.”
The Golborne team highlighted how community partnerships and culturally sensitive communication remain critical to ensuring that early diagnosis reaches every patient.
“It all starts with education,” said another clinician. “We saw what community groups achieved during the pandemic - those links still exist, but time is our biggest limitation.”

Facing the Pressures in Primary Care
The visit also revealed the realities of delivering proactive, preventative care in a high-demand urban setting. With limited space, the team frequently repurposes rooms - even corridors - to ensure every patient is seen. Expansion plans are already underway to increase clinical capacity next year. Despite these pressures, Golborne’s clinicians continue to innovate, integrating mental health support, opportunistic health checks, and early-diagnosis prompts into every consultation.
“Our patients work with us,” said a member of the Golborne team. “They know we’re doing our best - and they appreciate that.”
Partnership Beyond the Practice
Speaking after the visit, Joe Powell MP emphasised the importance of collaboration between community, technology, and health services:
“What’s happening here in Golborne - between GPs, community groups, and innovators like C the Signs - is exactly the kind of joined-up approach we need to deliver earlier diagnosis and better care.”
He also called for stronger links across the Integrated Care Board (ICB) and better alignment between voluntary and statutory services to tackle the wider determinants of health - from housing to mental wellbeing.
Dr Miles Payling, Co-Founder and Chief Scientific Officer at C the Signs, added:
“Early diagnosis begins in communities - in everyday conversations between GPs and patients, supported by technology that empowers those moments. Every 22 minutes, C the Signs helps detect another patient with cancer. What’s happening in Golborne shows how innovation can give patients back the one thing cancer takes away: time.”
Why It Matters
C the Signs was built by NHS doctors to work within existing systems and integrate seamlessly with primary-care workflows. Today, it is commissioned in over 1,500 GP practices, covering more than 10 million patient lives across the UK.
By enabling faster, more accurate triage and supporting clinicians at the point of care, the platform is redefining how cancer is detected - turning complex data into actionable insight and giving every patient a better chance of being seen in time.
Media enquiries
For press, interviews, or media information about C the Signs, please contact our PR team at cthesigns@moxiegrouppr.com

How does C the Signs work?
Early diagnosis changes lives. When cancer is found sooner, treatment can begin earlier and the chances of recovery improve. But recognising those early signs is rarely simple. In primary care, clinicians see a wide range of symptoms every day, many of which could point to something routine - or something more serious.
This is where supportive technology becomes essential.
Why early cancer symptoms are hard to recognise
Cancer doesn’t follow a single pattern. Two people with the same cancer can describe completely different symptoms - persistent tiredness in one person, back pain or bloating in another. With more than 100 cancer types and countless possible combinations of symptoms, it’s understandable that early detection can be challenging.
Primary care clinicians often have only a short window to explore concerns, manage records, and decide what needs further investigation. Guidelines can be detailed and complex, and symptoms often overlap with far more common conditions. Clinicians carry enormous responsibility. They deserve systems that help lighten that load.
How supportive technology can help
C the Signs was designed to give clinicians clear, timely insight when something might need a closer look. It draws together national guidance, clinical evidence, and local pathways to support decisions directly within existing primary care systems. It doesn’t replace clinical judgement - it strengthens it. Here’s how it supports the process:
Input
Clinicians enter symptoms, risk factors, concerns or test results directly within their usual systems.
Interpret
The platform analyses this information through validated pathways, clinical research and guideline recommendations.
Act
Within seconds, it offers a clear suggestion - whether that’s a referral, a specific test, or a safe next step - all tailored to the individual. All of this is inputted into the clinician's usual workflow. At present, we mostly work within the UK's National Health Service, and are actively used in over 25% of all practices.

Helping ensure patients are seen in time
Early diagnosis often relies on small details: a symptom that’s been lingering, a pattern that’s easy to overlook, or a concern that doesn’t quite fit. With clear prompts and structured follow-up, clinicians can monitor at-risk patients more easily and ensure those subtle signs aren’t lost between appointments.
This helps prevent delays that can happen when symptoms are unclear or when multiple conditions are being explored at once. It also supports safer safety-netting - making sure people return for the right checks at the right time. Every earlier diagnosis represents more time for treatment, more options, and more stability for patients and their families.
A more sustainable approach to early diagnosis
As pressures on primary care continue to grow, early cancer diagnosis must become more sustainable. Technology that works hand-in-hand with clinicians can support this by:
- reducing variation in care
- supporting consistent decision-making
- easing administrative burden
- helping identify patients who may otherwise be missed
- protecting referral pathways while improving accuracy
It’s a way of strengthening systems without increasing workload - and helping clinicians continue to deliver high-quality care under growing demand.
Working towards earlier diagnosis, together
Spotting cancer early will always be challenging. Symptoms rarely present neatly, and no single system or clinician can hold every pathway in mind during fast-paced appointments. That’s why supportive technology matters - not to replace people, but to ensure they’re equipped with the right information at the right time.
When clinicians are supported, patients benefit, and when patients are seen in time, outcomes change.
Early diagnosis starts with a single moment - a symptom mentioned, a pattern recognised, a decision made with confidence. Our role is to help make those moments easier to act on, so more people receive the care they need, when it can make the greatest difference.

Supporting primary care clinicians to diagnose cancer earlier
Diagnosing cancer early is one of the most complex and emotionally demanding responsibilities placed on primary care clinicians. It’s in primary care - the first place most people turn when something doesn’t feel right - where the earliest clues of cancer often appear. These signs are rarely clear, rarely dramatic, and rarely easy to separate from everyday illnesses.
And yet, this is where early detection begins. At the very first conversation. In the very first appointment. With the clinicians who know their patients best. This is why the demands placed on primary care clinicians are so great - and why they deserve systems designed to support them.
Seeing the small signs that can be easy to miss
In primary care, symptoms rarely arrive in neat, textbook patterns. Fatigue, a persistent cough, subtle abdominal discomfort, a quiet change in weight - these common concerns can be signs of countless conditions, most of them benign. But occasionally, they are the earliest indication of cancer.
Recognising these signals within a short consultation, often with partial information, is a profound clinical challenge.
Primary care clinicians must balance:
- large and growing patient caseloads
- time-limited appointments
- complex and evolving cancer guidelines
- administrative responsibilities such as referral coordination, documentation and safety-netting
- rising patient expectations and system pressure
And they must do so while ensuring every patient feels heard, reassured, and supported.
These pressures don’t simply affect workflows — they affect wellbeing. The emotional weight of worrying about a missed diagnosis can stay with clinicians long after their day ends.
Turning uncertainty into early action
Our platform analyses symptoms, risk factors, demographics, and clinical information in seconds - highlighting when a patient may be at risk and guiding the clinician toward the right next step.
It integrates within the systems clinicians already use, supporting healthcare teams across many regions, whether through EMIS, SystmOne or local electronic medical record systems.
This helps clinicians:
- Cross-check symptoms against validated cancer pathways
- Recognise rare or non-specific presentations earlier
- Refer or investigate patients with greater clarity and confidence
Every earlier investigation gives patients something invaluable: time to act, time to treat, and time to live the moments that matter.
Strengthening clinical judgment - not replacing it
Our platform is built to work with clinicians, never instead of them. It unites the best available evidence, national and international guidelines, and AI-powered insight in one clear, supportive view.
This leads to:
- Less diagnostic uncertainty
- More consistent, evidence-based decisions
- Improved patient safety and continuity of care
As one clinician shared:
“C the Signs helps me confirm when my instincts are right — and sometimes, when they’re not.
It ensures that no patient slips through the net.”
— GP, North West England
A global movement towards earlier diagnosis
Healthcare systems around the world share the same goal: to find cancer earlier and give patients the best possible chance.
Clinicians using C the Signs are already seeing meaningful change - with earlier referrals, faster diagnostic timelines, and improved identification of patients with cancer.
Behind every statistic is a person whose story is changed by earlier clarity. A family kept whole. A future rewritten.
Platforms like C the Signs - used across more than 1,500 practices and supporting over 10 million patient lives - help clinicians detect a patient with cancer every 22 minutes. Each one represents time given back.
More than technology - a partnership for better care
Technology alone doesn’t transform early cancer detection. People do.
Our platform is shaped hand-in-hand with clinicians across the world, grounded in their experience and continually refined through their insights.
Together, we’re helping shift early cancer detection from a reactive moment to a proactive standard of care - where every symptom is seen, every risk understood, and every patient given the best possible chance.
Image Credit: iStock

Why every moment matters: A message from Dr Miles Payling
At the inaugural C the Signs Conference, Dr Miles Payling - Co-Founder and Chief Scientific Officer - delivered a message that captured the heart of a movement reshaping how the world detects cancer.
He spoke about science, yes. But more importantly, he spoke about people. About time. About the moments we can give back when cancer is found sooner.
“We can’t afford to wait for symptoms to become obvious. Every moment matters - because every moment lost is a choice, a treatment, a life that could have been saved.”
The question that changed everything
Miles shared the story that shaped the mission behind C the Signs.
As an NHS doctor, he met a patient named Joe - active, fit, and 60 years old. After several GP (primary care) visits with vague symptoms, Joe arrived at hospital jaundiced and unwell. Scans confirmed metastatic pancreatic cancer.
Three weeks later, Joe died.
“Joe never asked, why do I have cancer? What he asked was, why was my cancer picked up so late?”
That question became the foundation of C the Signs - a platform built to help clinicians detect cancer early enough to change the outcome.
Today, that vision makes a measurable difference: a patient with cancer detected every 22 minutes.
Each one represents a life identified sooner - and a future that’s less defined by fear.
Why early detection still falls short
Cancer remains one of the leading causes of death worldwide. Survival still depends heavily on the stage at diagnosis.
- Breast cancer five-year survival falls from 97.9% at stage 1 to 26.2% at stage 4.
- Bowel cancer falls from 91.7% to 10.3%.
- Yet only around 58% of patients are diagnosed at an early stage.
In primary care - where most people first seek help - clinicians face enormous pressures:
brief consultations, complex presentations, thousands of patients, and on average only a handful of cancer diagnoses each year. As Miles said in his conference speech:
“The problem isn’t people. It’s knowledge. We need to give every GP the power of precision - instantly.”
Early detection doesn’t fail because clinicians aren’t trying.It fails because cancer is complex, symptoms are subtle, and the time to make sense of them is short. Our platform exists to bridge that gap - offering clinicians timely clarity when decisions need to be made.
Innovation and redefining what’s possible
C the Signs brings together trusted medical evidence, real-time data and AI-powered insight to support clinicians in moments where clarity matters most.
Within seconds, our platform can highlight when a patient may be at risk and guide their doctor toward the right diagnostic pathway - across more than 100 cancer types. But the impact isn’t defined by speed, it’s defined by the lives reached sooner.
Real-world evaluations across the NHS have shown that clinicians using C the Signs are able to:
- identify patients whose symptoms signal concern - even when the signs are hard to spot
- offer reassurance by safely ruling out risk when symptoms are more likely to be benign
- give clinicians clearer insight into where a tumour may have started
- help reduce emergency cancer presentations by half
- shorten the time it takes for patients to reach a diagnosis
Each of these outcomes represents something deeply human: a patient receiving answers earlier,
a family spared uncertainty, a healthcare system given space to care, not catch up.
This is what innovation should do - not stand in the place of clinical judgement, but enhance it. It should deepen insight and make the subtle more visible, so clinicians can act early with the confidence their patients deserve.
The movement, and honouring Jess’s Rule
Miles closed by sharing the story of Jessica Brady - a 27-year-old whose symptoms were subtle, persistent and easy to misinterpret. Despite several visits to her doctor, her cancer was found too late. Her loss is felt deeply, not only by those who loved her, but by clinicians across the country who want every patient to be seen in time.
To honour her legacy, our team is introducing Jess’s Rule - a safeguard within the platform that gently alerts clinicians when a patient returns multiple times with unresolved symptoms, prompting a thoughtful, timely cancer risk assessment.
It’s a small change with a profound purpose: to make sure no patient is ever unintentionally overlooked, and no pattern is missed simply because symptoms are subtle.
As Miles said:
“We can turn tragedy into transformation - by ensuring that no patient is ever overlooked again.”
Jess’s story is a reminder of why this movement matters. Together, we can help make early cancer detection a standard for everyone - not a privilege for a few - and give each person the time, choice and hope they deserve.
.webp)
How C the Signs integrates with EMIS and SystmOne to save lives
In primary care, time matters. Every consultation, every click, and every decision can shape a patient’s outcome - especially when it comes to cancer.
That’s why C the Signs has been designed to integrate seamlessly with EMIS and SystmOne, enabling GPs to detect cancer earlier without adding extra steps to their daily workflow.
Integration That Fits Naturally Into Primary Care
For most GPs, EMIS and SystmOne are the backbone of daily practice - holding every patient’s medical history, symptoms, and risk factors. C the Signs connects directly into these systems, transforming that information into real-time, actionable insight.
Through this integration, clinicians can:
- Instantly access C the Signs from within EMIS or SystmOne
- Automatically analyse patient symptoms, demographics, and clinical data
- Receive immediate, evidence-based guidance on cancer risk and next steps
No extra software. No switching screens. No duplicate data entry. Just faster, smarter decision-making - at the point of care.
Reducing the Time to Diagnosis
C the Signs is built to make early diagnosis simple, safe, and scalable. By embedding directly into the GP’s existing system, it eliminates delays that often occur when technology sits outside the electronic medical record.
This seamless workflow means:
- Referrals can be generated instantly, including under the Faster Diagnosis Standard (FDS), formerly known as the two-week wait (2WW).
- Patient data flows automatically, avoiding missed information or transcription errors.
- Audit trails and outcomes are logged for research, safety, and quality improvement.
In practices where C the Signs is live, clinicians are already finding cancer faster and more accurately - with earlier referrals, improved outcomes, and a reduced administrative burden.
Driving Early Diagnosis Across the NHS
C the Signs integrates directly with:
- EMIS Web - used by around 70% of GP practices in England
- SystmOne - supporting thousands of GP practices, community services, and hospitals
Together, these integrations make the platform available to millions of patients across the NHS — turning data into action and ensuring that every GP, regardless of location, has access to the same level of intelligent support.
Seamless, Safe, and Clinically Validated
Every integration is developed and maintained in line with:
- NHS Digital standards
- Clinical Safety DCB0129/0160 accreditation
- Information Governance and GDPR compliance
This ensures that C the Signs operates to the highest standards of clinical safety, patient privacy, and system performance — delivering technology clinicians can trust.
Real Impact, Real Patients
“The ability to use C the Signs directly in EMIS has completely changed how quickly I can act.
I can review a patient’s symptoms, get the cancer risk assessment instantly, and make the referral — all in one place.”
— GP, South East England
Every integration helps remove barriers between data and diagnosis - giving clinicians back time and patients back their best chance of survival.
About C the Signs
C the Signs is an AI-powered clinical platform that helps healthcare professionals identify patients at risk of cancer earlier, faster, and more accurately.
Founded by NHS doctors, the platform analyses over 100 cancer types using evidence-based algorithms and integrates directly into GP workflows through EMIS, SystmOne, and Vision.
By embedding early detection tools into everyday care, C the Signs is helping achieve the NHS’s ambition:
75% of cancers diagnosed at stage 1 or 2 by 2028.

Helping clinicians see the early clues with confidence
Spotting cancer early is one of the most meaningful moments in healthcare.
Yet it often begins with something small - a feeling that something isn’t quite right, a symptom that could easily be explained by everyday life, or a concern someone has carried for weeks before finding the courage to speak to a doctor. These early clues matter. But they can be incredibly hard to see.
When symptoms hide in plain sight
Many early signs of cancer are vague. Tiredness. A change in appetite. A persistent ache. Things almost everyone experiences at some point.
Clinicians across the world work within tight appointments, large caseloads, and complex diagnostic pathways. In the UK, this often means a doctor has ten minutes to listen, piece together a story, examine, review history, and decide whether more investigation is needed. In other health systems, the pressures look different, but the challenge is the same.
It’s easy to miss the early signals and it’s incredibly human to worry about missing something important.
The emotional side we rarely talk about
Early cancer detection is not just a clinical task - it carries emotional weight. Doctors want to offer reassurance, but they also want to act in time. Balancing those instinctive desires can be exhausting. Many share that the fear of overlooking something serious stays with them long after a consultation ends.
This pressure grows alongside administrative work: navigating referral pathways, coordinating tests, documenting every detail - all while trying to stay present for the next patient who walks through the door. This is why C the Signs exists: to do the heavy lifting in the background so clinicians can focus fully on the person sitting in front of them.
So what does that actually mean?
- Faster recognition of patients who may be at risk
- Clearer, more personalised diagnostic pathways
- More consistent follow-up and thoughtful safety-netting
- More time in appointments for human connection
Independent real-world evaluations have shown meaningful improvements, including fewer emergency cancer diagnoses and quicker routes to early-stage detection. At the centre of every data point is a person whose cancer was found earlier - and whose choices, time, and future were protected.
For clinicians, this support can ease the constant pressure. For patients, it brings earlier answers and a clearer path forward. For healthcare systems, it helps ensure early diagnosis becomes equitable and achievable for all.
Changing the story, one conversation at a time
Cancer is a disease of time - and every day gained matters.
We're just trying to help give some of that time back, transforming what is possible for millions of people and the clinicians who care for them.
.webp)
C the Signs launches womb cancer self-referral service
Somerset, UK - August 2024
C the Signs, in partnership with Somerset NHS Foundation Trust, is proud to announce the launch of a pioneering new self-referral service designed to transform the early diagnosis of endometrial (womb) cancer.
Using artificial intelligence, women over 50 can now complete a quick, evidence-based assessment - and if there is any indication of cancer risk, they are triaged immediately and booked in for an ultrasound scan.
This UK-first pathway is accelerating earlier and faster detection in post-menopausal women - a group at higher risk of developing endometrial cancer.
Transforming Access to Early Diagnosis
Endometrial cancer is one of the most common cancers affecting women in the UK, with over 9,700 new cases diagnosed each year. When found early, five-year survival rates reach 90%. In the latest stages, that drops to just 15%.
The new AI-powered self-referral pathway allows women experiencing post-menopausal bleeding or other symptoms of womb cancer to refer themselves directly for testing - without needing to contact their GP first.
This streamlined approach ensures faster access to diagnostic services and helps women get the right care at the right time.
A Clinically-Led Approach to Earlier Detection
“People will be able to get a diagnosis much earlier than before,”
said David Milliken, Consultant Gynaecological Oncologist at Somerset NHS Foundation Trust.
“We are seeing a year-on-year increase in referrals to our gynaecology cancer services, particularly for post-menopausal bleeding. By allowing patients to access our service directly via self-referral, we can avoid unnecessary delays and get them an appointment much more quickly.”
Dr Milliken added:
“This will also free up GP colleagues so they can see patients with other conditions. More than nine out of every ten women referred to our service will not have cancer. We hope this service will help to reassure the majority more quickly — and identify those who need treatment sooner.”
Empowering Women with Faster Access and Reassurance
Women’s health has long faced barriers to timely diagnosis and equitable care.
Helen Hyndman MBE, Ask Eve Nurse Service Co-ordinator at The Eve Appeal, praised the initiative:
“C the Signs’ self-referral service empowers patients by raising awareness of the symptoms of womb cancer and offering those experiencing post-menopausal bleeding a quicker appointment, closer to home. This will help provide reassurance and should increase the chances of womb cancer being diagnosed earlier, offering better outcomes.”
AI Innovation Driving a New Standard of Care
This initiative marks a significant step forward for women’s health - not just in reducing delays, but in empowering women with knowledge and faster access to life-saving diagnostics.
By simplifying the route to diagnosis, C the Signs and Somerset NHS Foundation Trust are setting a new national standard for how patients can access cancer diagnostic services across the NHS.
Dr Jude Gordon, Clinical Director at C the Signs, explained:
“At C the Signs, our mission is to break down barriers to earlier and faster cancer diagnosis. By enabling women to take control of their health and assess their symptoms, we’re ensuring faster access to specialist services and the right care at the right time - increasing the chances of surviving cancer.”
Scaling Early Detection Across the NHS
This pathway is the first of several AI-enabled self-referral services being launched across the NHS.
C the Signs will soon expand the model to include pathways for colorectal (bowel) and lung cancer, furthering its mission to make early detection a standard for all, not a privilege for some.
Together with Somerset NHS Foundation Trust, C the Signs is advancing women’s health, improving equity of access, and giving more people the time and opportunity that early diagnosis provides.
Contact
To learn more about how C the Signs can accelerate cancer diagnosis in your region,
contact hello@cthesigns.com or visit cthesigns.com

How Princess Kate’s bravery is shifting cancer awareness
In the wake of Princess Kate's deeply personal revelation, disclosed amidst relentless scrutiny from the press following her absence from royal duties, we are reminded of the delicate balance between public life and private suffering.
Her disclosure, shared with a heavy heart, was not a choice freely made but a response to an untenable situation where the boundary of personal privacy was breached by widespread speculation. Princess Kate demonstrated unparalleled bravery and a profound sense of solidarity with those quietly enduring their battles with cancer.
This situation underscores a critical conversation about the sanctity of privacy and the broader implications for everyone navigating through a cancer diagnosis. The loss of privacy can often feel like a loss of control, a sentiment deeply resonant with those dealing with cancer. It eliminates the autonomy to choose how and when to confront one's vulnerabilities, adding an unnecessary burden during an already tumultuous time. Respecting someone's diagnosis means allowing individuals the dignity to face their illness on their terms, to maintain control over their narrative, and to protect their identity from being overshadowed by their diagnosis.
The forced unveiling of Princess Kate's cancer diagnosis highlights the intense pressure public figures often face, transforming what should be a deeply private matter into public discourse. However, the manner in which she chose to address this unwelcome spotlight offers us a moment for reflection and, ultimately, inspiration.
The revelation of her diagnosis at the age of 42, as a mother of three, challenges widespread misconceptions about who can be affected by this pervasive disease. It underscores the stark reality that 1 in 2 individuals will face a lifetime risk of cancer, with 1 in 10 new diagnoses occurring in the 25-49 age group, and women being twice as likely as men to be diagnosed within this bracket. These statistics highlight the indiscriminate nature of cancer and emphasise the critical need for increased awareness and early detection efforts.
By sharing her story, Princess Kate has built a bridge of solace and understanding with women, parents, and cancer patients everywhere, those who grasp the depth of her experience on a profoundly human level. It serves as a reminder that behind the titles, responsibilities, and expectations are individuals grappling with their vulnerabilities, fears, and the daunting journey of cancer treatment. The princess's situation underscores why many opt to navigate their illness in private—protecting not just their sense of self but also affording themselves the space to cope with the multifaceted challenges cancer brings without the additional burden of public scrutiny.
Princess Kate's openness serves as a rallying cry for solidarity and hope. It's a poignant reminder that cancer does not discriminate—it can affect anyone's life, regardless of age or status. Her courage in sharing her story should serve as a call to action, urging people to actively engage in their health by recognising symptoms, understanding risks, and promptly seeking medical advice when needed, thus offering an opportunity to demystify the disease and encourage open discussions about health and the importance of early detection.
As our hearts go out to Princess Kate and countless others on their personal cancer journeys, this moment invites us to reflect on the compassion, understanding, and respect we owe to one another, fostering a community where everyone feels supported in their time of need.
References:
Cancer Research UK - almost 10% of new cancer diagnoses in people aged 25-49
NHS - 1 in 2 people will get cancer at some point in their lifetime

C the Signs launches across 70 GP practices in Dorset ICS
In partnership with NHS England’s InHIP Programme, Dorset Integrated Care System Cancer Programme, NHS Dorset, and Health Innovation Wessex, the C the Signs Cancer Clinical Decision Support System has now been launched across all 70 GP practices in Dorset - marking a major step forward in the region’s efforts to detect cancer earlier and improve survival outcomes.
Transforming Cancer Diagnosis Across Dorset
Dorset’s population has one of the highest rates of cancer in the UK, with its older demographic particularly vulnerable to late diagnosis.
When cancer is found early, lives can be transformed - for example, over 90% of patients survive colorectal cancer for five years or more when diagnosed early, compared to less than 10% when detected late.
By supporting GPs to identify at-risk patients at the earliest possible stage, C the Signs is helping to ensure that every patient in Dorset has an equal chance of earlier detection and better outcomes.
Reducing Inequalities, Increasing Access
Working in alignment with NHS England’s Core20PLUS5 approach to tackling healthcare inequalities, this partnership focuses on raising awareness, increasing community engagement, and ensuring equitable access to cancer diagnostics - particularly in areas of high deprivation.
The rollout is part of the InHIP (Innovation for Healthcare Inequalities Programme), designed to reduce variation in access to care and improve outcomes across the country.
“One of our key priorities is to add healthy life years to people living in Dorset, and early detection of cancer symptoms is key to achieving this.
When caught early, survival rates are greatly improved - and we are confident C the Signs will help us realise that ambition.”
- David Freeman, Chief Commissioning Officer and Deputy Chief Executive, NHS Dorset
Empowering Clinicians, Enabling Earlier Diagnosis
The C the Signs platform integrates directly with GP systems, including EMIS and SystmOne, analysing patient symptoms, risk factors, and medical history to help GPs identify potential cancer risk in under 30 seconds.
By supporting decision-making at the point of care, the platform is helping to reduce missed diagnoses, speed up referrals, and ensure patients access the right tests and pathways sooner.
This initiative is another step towards making early diagnosis the standard - not the exception - across the NHS.
A Shared Mission
“We’re proud to partner with NHS Dorset, Health Innovation Wessex, and NHS England’s InHIP programme to bring our platform to every GP practice in the region.
Together, we’re working to ensure every patient - regardless of where they live - has the best possible chance of surviving cancer.”
— Dr Bea Bakshi, Co-Founder and CEO, C the Signs
Driving Impact Across the NHS
C the Signs is now used by over 10,000 healthcare professionals across 1,500 GP practices, helping detect a patient with cancer every 22 minutes and supporting early detection across more than 100 cancer types.
By combining AI, clinical evidence, and national cancer pathways, C the Signs continues to redefine what’s possible in cancer detection - giving patients back time, choice, and hope.
📖 Read the full article on HSJ: www.hsj.co.uk
📩 Contact us at hello@cthesigns.com to learn how C the Signs can accelerate early cancer diagnosis in your region.
Image Credit: iStock

How C the Signs is transforming early cancer detection in the UK
At C the Signs, we believe no one should face a late cancer diagnosis.Our mission is clear and urgent - to empower every GP to detect cancer earlier and give every patient the best chance of survival.
Why We Started
Every two minutes, someone in the UK is diagnosed with cancer. For too many, it’s discovered too late - when options are fewer, outcomes are poorer, and lives are changed forever.
The challenge isn’t a lack of care or compassion - it’s the complexity of cancer itself. With over 100 cancer types and countless symptom combinations, even the most experienced GP can face uncertainty during those vital early consultations.
C the Signs was born from a single question:
“What if technology could help doctors spot the earliest signs of cancer - before it’s too late?”
That question became our why - and our purpose.
What We Do
C the Signs is an AI-powered clinical platform that helps healthcare professionals identify patients at risk of cancer - earlier, faster, and more accurately.
Our technology integrates directly with NHS electronic medical record systems like EMIS, SystmOne, and Vision, analysing combinations of:
- Signs and symptoms
- Risk factors and clinical markers
- Demographic and lifestyle data
Using validated algorithms and national evidence-based pathways, C the Signs supports GPs to assess cancer risk and identify the most appropriate referral or diagnostic route - in under 30 seconds.
The result: fewer missed cases, faster investigations, and more lives given back time.
How It Works
C the Signs combines artificial intelligence, clinical research, and national guidelines to transform medical decision-making.
- Analyse – The platform reviews real-time patient data and symptom inputs.
- Assess – AI cross-checks patterns against validated cancer pathways and the latest clinical evidence.
- Act – GPs receive instant, tailored guidance on next steps - from urgent referrals to diagnostic tests.
By translating complex data into clear, actionable insights, C the Signs enables clinicians to make faster, more confident decisions - while maintaining full clinical autonomy.
Our Impact So Far
C the Signs is now used across the UK by over 10,000 healthcare professionals in 1,500 GP practices, helping identify patients with cancer every 22 minutes.
Validated through independent evaluations and peer-reviewed studies, the platform has shown:
- 99% sensitivity for identifying patients with cancer
- 99% negative predictive value, safely ruling out risk
- 94% accuracy in predicting tumour origin
- Stage shift in harder-to-detect cancers such as pancreatic and ovarian
- Faster time to diagnosis, reducing delays by over 20%
- More equitable detection, with fewer emergency presentations and earlier referrals across diverse populations
Every earlier diagnosis represents more time - and more life - for patients and their families.
The Team Behind the Mission
C the Signs was founded by Dr Bea Bakshi and Dr Miles Payling, two NHS doctors who saw firsthand how late diagnosis can cost lives.
Their experience on the frontline of care inspired a bold vision: a future where technology and medicine work together to make early cancer detection the norm — not the exception.
Today, our multidisciplinary team of clinicians, data scientists, and innovators share one purpose:
to end late cancer diagnosis, for good.
A Future Without Late Diagnosis
Our journey is just beginning.
We’re continuing to advance our AI, expanding across care settings - from primary to secondary care and beyond - to make early cancer detection universal and equitable.
Through partnerships with Cancer Alliances, Health Innovation Networks, and NHS England, we’re shaping a future where no symptom is overlooked and no patient waits too long to be seen.
Our vision is bold, but achievable:
A world where no patient is diagnosed too late.
Join Us
Whether you’re a GP, policymaker, or innovation partner - together, we can rewrite the story of cancer care.
👉 Learn more about our research and impact.
👉 Request a demo to see how C the Signs integrates with your NHS system.
👉 Join our mission to make early detection a standard for all.

Does masturbation increase my risk of prostate cancer?
Prostate cancer remains one of the most common cancers in men, and one of the most survivable when it’s found early. Over the years, there’s been widespread interest in whether sexual activity, including masturbation or ejaculation frequency, might influence prostate cancer risk.
The short answer: research suggests there may be a link, but it’s more complex than it seems.
What the research shows
The idea that ejaculation could affect prostate cancer risk comes from long-term population studies, rather than direct clinical trials. These studies don’t prove cause and effect, but they do reveal patterns worth exploring.
Early studies
In 2009, a UK study (Dimitropoulou et al.) suggested that frequent masturbation in younger men (in their 20s) might be linked to a slightly higher risk of prostate cancer later in life, while frequent masturbation in older men (in their 50s) appeared to be protective.
Researchers proposed that younger men with high testosterone, and therefore higher libido, might already have a greater biological risk due to hormone sensitivity, rather than the act of masturbation itself.
More recent evidence
A larger US study published in European Urology (Rider et al., 2016) followed more than 30,000 men over 18 years. It found that men who ejaculated at least 21 times per month had a 20% lower risk of being diagnosed with prostate cancer than those who ejaculated 4-7 times per month.
The association was strongest for low to moderate grade prostate cancers, suggesting that more frequent ejaculation could play a role in keeping the prostate healthy - potentially by clearing out harmful substances or reducing inflammation.
Another analysis published in 2017 in The Journal of Sexual Medicine (Papa et al.) found that men who had higher ejaculation frequency in their 30s were less likely to develop advanced prostate cancer later in life, although the effect was modest and not seen in all age groups.
More recent meta-analyses (through 2022–2024) have continued to support the idea that ejaculation frequency may offer a small protective effect, but they agree that the evidence remains observational, not causal (Kokori, 2024).
Why might ejaculation help?
Researchers have proposed a few possible explanations:
- Reducing inflammation: Regular ejaculation may help flush out potentially harmful substances or reduce inflammation in the prostate.
- Regulating cell turnover: Ejaculation could help keep cell metabolism stable, reducing opportunities for abnormal cell growth.
- Hormonal balance: Regular sexual activity may help maintain a steady balance of androgens (male sex hormones), which are known to influence prostate cancer risk.
But there’s still no definitive proof. These findings show correlation, not cause - meaning that men who ejaculate more frequently might also lead generally healthier lifestyles.
What does this mean for patients and clinicians?
There’s no medical recommendation for ejaculation frequency as a form of prostate cancer prevention.
However, the evidence is reassuring:
- Masturbation and sexual activity are safe and normal parts of life.
- There’s no evidence that they increase risk at any age.
- Prostate cancer risk is more strongly linked to age, family history, ethnicity, and genetics than to sexual habits.
Encouraging men to understand their risk, attend screening when eligible, and act on new or unusual urinary symptoms remains the best way to protect health.
The takeaway
Ejaculation may have a small protective role in prostate health, but it’s not a proven way to prevent cancer. What we do know is that:
- Early detection saves lives.
- Regular health checks and awareness of changes matter more than any single lifestyle factor.
- Masturbation and sexual activity are healthy and safe.
Prostate cancer caught early is highly treatable. Empowering people with knowledge, not fear, is how we give them back time, choice and life.
References
Dimitropoulou, P., Lophatananon, A., Easton, D., et al. (2009). Sexual activity and prostate cancer risk in men diagnosed at a younger age. BJU International, 103(2), 178–185.
Rider, J. R., et al. (2016). Ejaculation frequency and risk of prostate cancer: updated results with an additional decade of follow-up. European Urology, 70(6), 974–982.
Papa, N. P., MacInnis, R. J., English, D. R., Bolton, D., Davis, I. D., Lawrentschuk, N., Millar, J. L., Pedersen, J., Severi, G., Southey, M. C., Hopper, J. L., & Giles, G. G. (2017). Ejaculatory frequency and the risk of aggressive prostate cancer: Findings from a case-control study. Urologic oncology, 35(8), 530.e7–530.e13. https://doi.org/10.1016/j.urolonc.2017.03.007
Kokori, Emmanuel & Olatunji, Gbolahan & Isarinade, David & Aboje, John Ehi & Ogieuhi, Ikponmwosa & Zainab, Doyinsola & Lawal, Abera & Woldehana, Muhammad & Nazar, & Godfred, Yawson & Scott, Nicholas & Aderinto, & Lawal, Zainab & Woldehana, Nathnael & Nazar, Muhammad Wajeeh & Scott, Godfred & Aderinto, Nicholas. (2024). Ejaculation Frequency and Prostate Cancer Risk: A Narrative Review of Current Evidence. Clinical Genitourinary Cancer. 10.1016/j.clgc.2024.01.015.

Elevating the role of nurses in early cancer detection
On 9 September 2025, C the Signs and the Royal College of Nursing (RCN) co-hosted a pivotal webinar titled “The role of primary care nurses in early cancer diagnosis.” The Royal College of Nursing in bringing together nursing professionals, primary care leaders, and clinical innovators, the event made clear that earlier detection of cancer is not just about tools - it’s about people, processes, and partnership.
Why this webinar mattered
- A vital gap to fill. Almost half of cancers in the UK are still diagnosed at a late stage, when treatment is less effective. The Royal College of Nursing In primary care, symptoms are frequently vague or non-specific - meaning the margin for error is narrow, and the cost of delay is high.
- Nurses are central. Whether as practice nurses, advanced nurse practitioners, healthcare assistants, or part of the wider team, nursing staff are often the first to see patients, triage symptoms, and coordinate care escalation. This webinar affirmed their critical role in recognising risk, escalating appropriately, and helping patients navigate diagnostics.
- Digital support can change outcomes. The session introduced how clinical decision support systems - like C the Signs - can augment clinical vigilance, helping teams to assess cancer risk faster, more consistently, and more equitably.
What the webinar covered
The agenda was structured to bridge theory and practice. Key themes included:
- Challenges of early diagnosis in primary care - recognising “red flags” and patterns when symptoms are ambiguous.
- NICE cancer guidelines in real life - translating guidance into day-to-day decisions.
- Case studies - including FIT (faecal immunochemical test), PSA, cervical screening, post-menopausal bleeding, and more.
- Team roles & escalation - how every member of the practice team contributes to spotting and acting on cancer risk.
- Clinical decision support in action - how platforms like C the Signs streamline assessment, flag risk, and suggest appropriate referral pathways.
- Interactive Q&A - giving attendees a chance to probe, challenge, and learn.
What this means in practice
The webinar reaffirmed a powerful shift: early cancer detection will increasingly be achieved not by siloed brilliance, but by connected teams working with intelligent augmentation.
- Nurses become more empowered to act on subtle cues, supported by systems that help flag risk early.
- Diagnostic pathways get activated sooner, shortening the time between suspicion and investigation.
- Inequalities may shrink: consistent decision support helps reduce variation in care across regions and teams.
This aligns with the real-world impact C the Signs is already showing. In GP practices using the platform, cancer detection rates have improved (for example, a jump from 58.7 % to 66.0 % in a study of 35 practices) - doing so without burden to the clinicians.
Voices from the session
One comment from the live discussion echoed what many already believe:
“Even when symptoms don’t look classic, having a prompt or nudge helps us check further rather than wait.”
That underscores exactly why combining human expertise with AI is transformative - we don’t replace intuition or experience, we sharpen and scale them.
Looking ahead: how to make this real
To turn the insights from the webinar into frontline change, we need action:
- Embed tools in everyday workflows. Decision support systems must feel seamless - integrated into existing electronic record systems, not a bolt-on.
- Invest in training & trust. Clinicians need confidence in AI, through education, demonstration, and peer support.
- Track outcomes & learning. Monitor how decision tools affect referral patterns, stage at diagnosis, and equity across populations.
- Champion policy & resource alignment. Systemic support - from commissioners, health systems, and regulators - is essential to scale early detection equitably.
Rewriting what’s possible
The RCN – C the Signs Webinar wasn’t just another educational event - it was a statement of purpose. It reaffirmed that nurses are pivotal to rewriting cancer’s timeline. It showed us that technology, when built with care and aligned to workflow, can restore precious time to patients. And it made clear that early detection is not a dream - it’s an imperative we can deliver together.
At C the Signs, our mission is to give people back time, choice, and life through earlier, safer, more equitable diagnosis. That mission comes alive when we partner with frontline clinicians - and this webinar is just one step in the journey. The transformation is underway, and we’re leading it together.

Do sunbeds give a false sense of safety?
Sunbeds are often promoted as a “controlled” way to tan, a chance to build colour gradually and avoid burning on holiday. On the surface, it sounds like a sensible option.
But science tells a different story.
There’s no such thing as a safe tan from a sunbed. The idea that tanning under UV light can protect your skin later on is a comforting myth, one that’s left many people unknowingly at risk.
The myth of protection
A tan isn’t protection, it’s proof that your skin has been working hard to defend itself. That change in colour is your body’s signal that it’s already had too much UV exposure.
Research shows that using a sunbed before 35 increases the risk of melanoma by up to 59%.
Melanoma is one of the most serious forms of skin cancer, but when detected early, around 90% of people survive (Cancer Research UK). That’s why awareness and timely detection are so important.
Sunbeds don’t build protection, they build exposure.
Why this belief persists
For years, sunbeds have been described as “controlled UV.” The message has been that a few short sessions are safer than natural sunlight. In reality, the UV rays from a tanning bed can be up to six times stronger than the midday Mediterranean sun. Even one session can damage the DNA inside skin cells - the code that controls how they grow and repair. When that damage builds up, it can cause cells to grow abnormally and form cancer.
Why it matters now
In October 2025, leading dermatologists and cancer experts urged the UK Government to follow Australia’s example and ban commercial sunbeds altogether. Their call was supported by research published in the BMJ, which concluded that an immediate, outright ban on commercial sunbeds, combined with public education, is the most cost-effective way to reduce skin cancer, save lives and ease pressure on the NHS (Kreft et al., 2025).
Countries such as Australia, Brazil and Iran have already implemented bans after clear evidence linked tanning beds to melanoma. Experts argue that with melanoma rates still rising in the UK, similar action here could prevent thousands of avoidable cancers each year (Kreft et al., 2025).
This isn’t a debate about personal choice; it’s about ensuring everyone has the same opportunity to make informed decisions, free from misinformation or risk. Education and prevention save lives long before treatment is ever needed.
What you can do
You don’t have to give up how tanning makes you feel to stay safe. There are simple, healthy alternatives:
- Choose sun-free glow: Self-tan lotions and sprays give the same colour without UV exposure.
- Protect your skin: Use SPF 30+ daily, even in the UK. Wear a hat and stay in the shade when the sun is strongest.
- Know your skin: Check regularly for new moles or changes. If something looks different, speak to your GP - early detection saves lives.
- Share the message: Talking about tanning myths helps others make informed choices too.
The takeaway
Sunbeds may feel safe because they’re familiar, controlled and easy, but they aren’t harmless. Knowing the truth isn’t about fear, it’s about freedom: the freedom to choose options that protect your skin and your future.
Every moment of awareness, every early detection, every informed choice gives people back time, choice and life.
References
https://www.bmj.com/content/391/bmj-2025-085414
https://www.cancerresearchuk.org/get-involved/campaign-for-us/all-our-campaigns/sunbeds











.svg%201.png)
